Among its notable accomplishments, Autoimmune Registry (ARI) was cited in the National Academy of Sciences for our comprehensive list of autoimmune diseases and classification by level of evidence. ARI was also featured by the National Institute of Health's All of Us program for our work analyzing health-related data to better understand autoimmune diseases.
What is the connection between autoimmune diseases and cancer?
Many of us have heard that our autoimmune diseases put us at an increased risk for cancer, but what is the connection between cancer and autoimmune diseases? The two are similar in that they can both involve dysfunctions of the immune system. Cancer often develops when our immune system fails to attack defective cells. On the other hand, autoimmune diseases develop when our immune system is overactive and attacks our own cells.
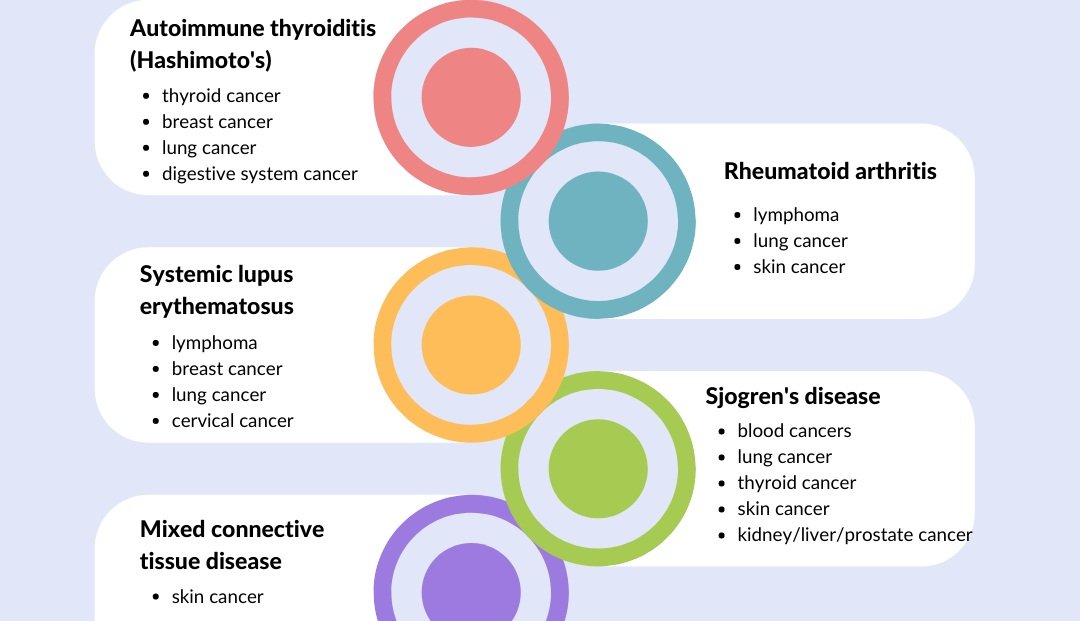
Firstly, autoimmune diseases can lead to chronic inflammation, which is a risk factor for cancer. Patients with autoimmune diseases that attack specific organs will be at an increased risk of developing cancer in those organs. For example, patients with Crohn's disease, Celiac disease, or ulcerative colitis are at an increased risk for colorectal cancer, and patients with pernicious anemia or autoimmune gastritis are at higher risks of developing gastric cancer. Below are a few known associations of common autoimmune diseases in our registry and cancer risks:
Secondly, certain medications taken by patients with autoimmune diseases may put the patients at an increased risk for cancer. In particular, immunosuppressants turn off a part of the body's immune system, and thereby reduce the body's ability to destroy cancerous cells.
Finally, certain cancers and cancer treatments can cause autoimmune diseases. When the immune system attempts to fight off the cancer cells, it can become too active and develop autoimmunity. For example, patients with leukemias and lymphomas can develop warm autoimmune hemolytic anemia. Certain cancer treatments like immunotherapy, which activates the immune system to attack cancer cells, can also cause autoimmune diseases as a side effect.
All of these risks were identified through studies of subsets of the patient population. What other connections can we find when we have more data on autoimmune disease patients? This is why it's so important to have a centralized autoimmune disease registry. Like the National Cancer Registry, ARI wants to be able to forecast autoimmune disease patients' likely outcomes. Please help us achieve this by joining our registry and sharing our information on social media. Donations are also greatly appreciated!
Sources:
Hashimoto's: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9318815/
Rheumatoid arthritis: https://www.rheumatologyadvisor.com/home/topics/rheumatoid-arthritis/rheumatologists-cancer-risk-management-patients-with-rheumatoid-arthritis/
Lupus: https://www.hopkinslupus.org/lupus-info/lifestyle-additional-information/lupus-cancer/
Sjogren's: https://sjogrenssyndromenews.com/news/analysis-finds-increased-risk-cancer-sjogrens-syndrome-patients/
Mixed connective tissue disease: https://www.hmpgloballearningnetwork.com/site/autoimmune/web-content/connective-tissue-diseases-associated-increased-risk-nonmelanoma-skin-cancer
Is fibromyalgia an autoimmune disease?
One of the most commonly reported conditions by our registrants is fibromyalgia (fibro). This condition has long baffled physicians with unexplained pain and fatigue reported by patients. One study published in 2021 found evidence that fibro may be autoimmune.
When scientists injected a type of antibody called IgG from fibro patients into mice, they detected hypersensitivity to pressure and cold stimulation among the mice. In contrast, mice injected with IgG from healthy subjects had no such sensitivity. The study concluded that IgG from fibro patients produced painful sensory hypersensitivities and that therapies aimed at reducing these antibodies may be effective for fibro.
Over 500 people in the Autoimmune Registry (ARI) reported having fibro. Among these individuals, almost 98% reported having another autoimmune condition. Below is a breakdown of the top confirmed autoimmune diseases reported by fibro patients in our registry
It is possible that fibro is an autoimmune disease, but more research is needed to determine the immune mechanisms at work. ARI supports this research, which we believe will lead to improved diagnosis and treatments.
Help us learn more about autoimmune diseases by asking others with the diseases to join our registry. Donations are also greatly appreciated! Together, we can better uncover the connections among autoimmune diseases.
Can microbiomes in our gut lead to rheumatoid arthritis?
We've long suspected a connection between the immune system and our gut. In fact, many of us with autoimmune diseases develop food sensitivities to foods like gluten and dairy.
Scientists have now identified a bacteria that is only found in the intestines of people with rheumatoid arthritis and not in healthy individuals—Subdoligranulum didolesgii. Moreover, when scientists gave oral doses of the bacteria to mice, they found that the mice began to develop joint swelling and antibodies attacking the joints within 14 days.
Many immune responses naturally occur in the intestines, with our immune system attacking the microbiome to maintain balance of the good and bad bacteria. These immune responses have usually been contained in gut, with a "firewall" that prevents the antibodies from bypassing the intestines.
Scientists hypothesize that a particularly strong intestinal immune response against this particular bacteria may have somehow spread beyond the intestines to other parts of the body. Once outside of the intestines, the antibodies for the bacteria then trigger an immune attack against the joints, leading some people to develop rheumatoid arthritis.
The more we learn about the origins of autoimmune diseases, the more potential paths we have to discovering a treatment. To support the Autoimmune Registry, please register and share our mission with others who have autoimmune diseases. Donations are also greatly appreciated!
Experiences with biologic treatment
Last time, we wrote about biologic treatment and asked about your experiences. We're publishing a few of the responses below, with names and dates removed to protect anonymity.
“Rituxan saved my life. I get 2 infusions, two weeks apart every six months. At first I really didn’t want to pump the strong medication into my body, but by the 4-5 months I am begging for it. It has truly given me some sort of life back.
”
“My daughter became sick and tried most available pharmaceutical treatment options for mixed/undifferentiated connective tissue disease. She was in lots of pain and not growing or thriving. We started the biologic Orencia and it has been a miracle. She started gaining weight, growing and her pain was so much better after a few months. She now has a monthly infusion.”
“A year after a diagnosis of CHAD (Cold Hemolytic Anaemia Disease) I was given a course of 4 doses of Rituximab. This improved my blood count from around 70 to around 90. I then received a diagnosis of non-Hodgkin-lymphoma. My blood count has fluctuated since (in the 80s) but I haven’t needed a second Rituximab treatment.”
“I have a TRAPS variant autoimmune disorder and have taken Kineret (Anakinra) by injection, 100mg, up to twice a day, for 5+ years. It completely arrests any flare and my doctors think regular use keeps flares from happening. Do I love the injections? Of course not. But they have given me back my life. I don’t have any side effects, really.”
What else would you like to see in our newsletters? Send us your suggestions through our contact form.
How did we inherit our autoimmune diseases?
We've long known there is a genetic component to autoimmune diseases. Autoimmune diseases tend to run in the family, suggesting that certain genes make us more likely to develop the diseases. But how did these genes evolve and why does it seem like more and more people are being diagnosed with autoimmune diseases today?
A geneticist found that a set of genetic variants which once protected our ancestors from the plague may now be increasing our risks for autoimmune diseases. These gene variants boost the body's immune response to the bacteria that caused the plague, but they are also associated with higher risks of autoimmune diseases.
During the Black Death plague, people with just one of the gene variants were 40% more likely to survive the plague than those without the variant. As a result, after the plague eradicated a large percentage of the population in the 1300's, those who survived were much likely to have the gene variants.
Today, many of us may have inherited these variants. By learning more about the origins of autoimmune diseases, we hope to better understand and, one day, successfully treat autoimmune diseases.
To support the Autoimmune Registry, please join here or share it with your advocacy or support group. Donations are also greatly appreciated!
Alzheimer's as an autoimmune disease
Alzheimer’s is the most familiar form of dementia. Though we are all familiar with autoimmune brain fog, scientists have not previously made the connection between Alzheimer's and autoimmune disease.
It was well known that the protein involved in Alzheimer’s is beta-amyloid, but the protein was previously viewed as an anomaly that shouldn't be in the brain. Recently, however, scientists from the Krembil Brain Institute published a study that found Alzheimer's to be an autoimmune disease of our innate immunity.
““We don’t think of Alzheimer’s as fundamentally a disease of the brain. We think of it as a disease of the immune system within the brain.””
The study found beta-amyloid to be a part of our body's innate response to injury or infection. When it is released in patients with Alzheimer's, it mistakenly attacks the body's own neurons (because of surface similarities between the neurons and bacteria). The destruction of the neurons then leads the body to continue to believe that it is under attack and release more beta-amyloid in response, resulting in a perpetuating cycle of chronic attacks to the brain's own neurons.
The finding that beta-amyloid is autoimmune has opened new doors of opportunity for the management and treatment of Alzheimer’s disease. Perhaps, one day, this line of research will also lead to more insights and treatments for brain fog.
At the Autoimmune Registry, we are gathering epidemiological data on all autoimmune diseases to build a more complete picture of this disease class. You are a vital part of our mission to better understand autoimmune diseases. Please join our registry and share it with others who have autoimmune diseases. Donations are also greatly appreciated!
Can Covid trigger the onset of autoimmune diseases?
Previously, we wrote about long Covid being a suspected autoimmune disease. But there have also been reports of patients developing autoimmune diseases after they've recovered from Covid.
One of the ways this can happen is called "molecular mimicry." When a virus attacks our body, the body generates antibodies that bind to the surface of the virus. These antibodies then signal our immune system to attack the cells they're attached to. When proteins on the surface of a virus looks similar to the normal proteins in our body or organs, the antibodies will sometimes mistakenly bind to our own body, causing autoimmunity.
Some of the autoimmune antibodies that have emerged from people with severe Covid include those associated with lupus, rheumatoid arthritis, Guillain-Barre syndrome, immune thrombocytopenia, and autoimmune hemolytic anemia. Did you develop an autoimmune disease after contracting Covid? We'd love to listen to and share your story. Contact us here.
Please join our registry or share it with your local advocacy group. Donations are also greatly appreciated. Together, we can better understand autoimmunity!
Does gene therapy offer a solution for autoimmune diseases?
With better understanding of our genomes, scientists have increasingly looked to personalized medicine or gene therapy to target diseases. Recently, gene therapy was used to effectively treat 5 lupus patients in a ground breaking study.
The technology used is called CAR T-cell therapy. T cells are our body's immune cells that help fight off infections and destroy cancer cells. Traditionally, CAR T-cell therapy has been used to fight cancer. A patient's blood is drawn to isolate the T cells, which are then genetically modified to attack the cancerous tumor cells. When the T cells are reinjected into the patient's body, the modified T cells have helped cancer patients achieve remission.
Recently, scientists used the same CAR T-cell technology to modify T cells to attack B cells, which create antibodies. In patients with autoimmune diseases like lupus, B cells incorrectly produce antibodies that signal the body to attack its own cells. In this study, when patients were injected with the modified T cells, their B cells completely disappeared in a few days and the patients' symptoms improved.
But what is more incredible is that, after a few months, when B cells began to grow back, they did not produce the defective antibodies that previously led to lupus activity. The immune system had effectively reset itself, and the study patients continued to be in drug-free remission 8 to 12 months after the treatment. This opens up a whole new avenue for exploring treatments for autoimmune diseases. However, this type of personalized gene therapy is still very expensive today.
What topics would you like to see in our next newsletter? Let us know and we will try to publish a newsletter on your topic of choice.
Support like yours is so important to our organization. Please join our registry or share it with friends who have autoimmune diseases. Donations are also greatly appreciated.
The most common autoimmune disease symptoms (based on 196 survey results)
Last week, we posted a Facebook poll results from our Multiple Autoimmune Syndrome group, providing the percentage of votes for each symptom. In that email, we also shared a link to fill out a survey on diseases, symptoms, and medications, and the results are in! With the survey, we can link the symptoms to individual survey IDs and their reported diseases.
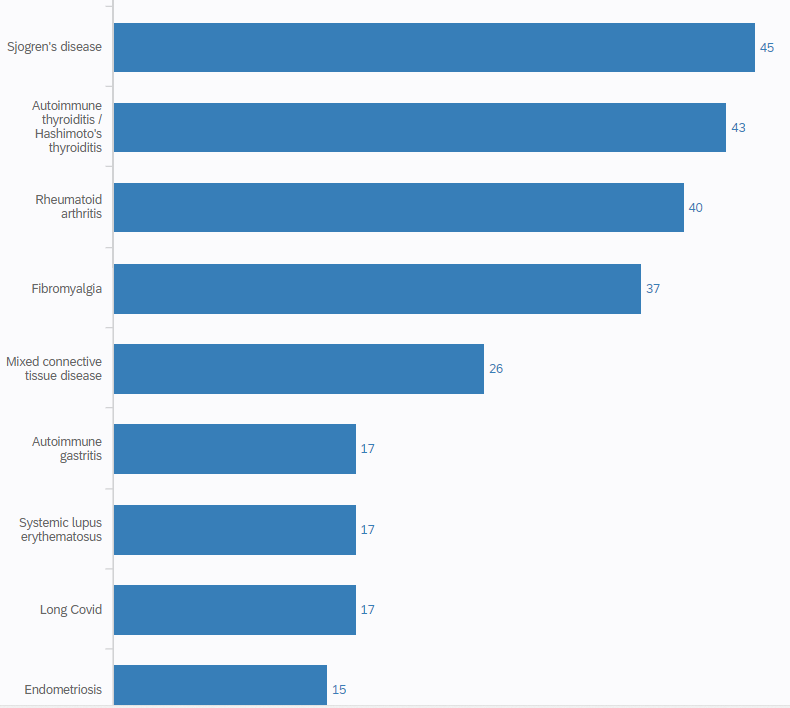
Based on 196 anonymous surveys from patients that reported over 65 different autoimmune diseases, 147 reported having more than 1 autoimmune disease. The most common autoimmune disease reported in this survey is Sjogren’s disease, followed by Hashimoto’s or autoimmune thyroiditis, and rheumatoid arthritis. Below is a list of the diseases with the most counts.
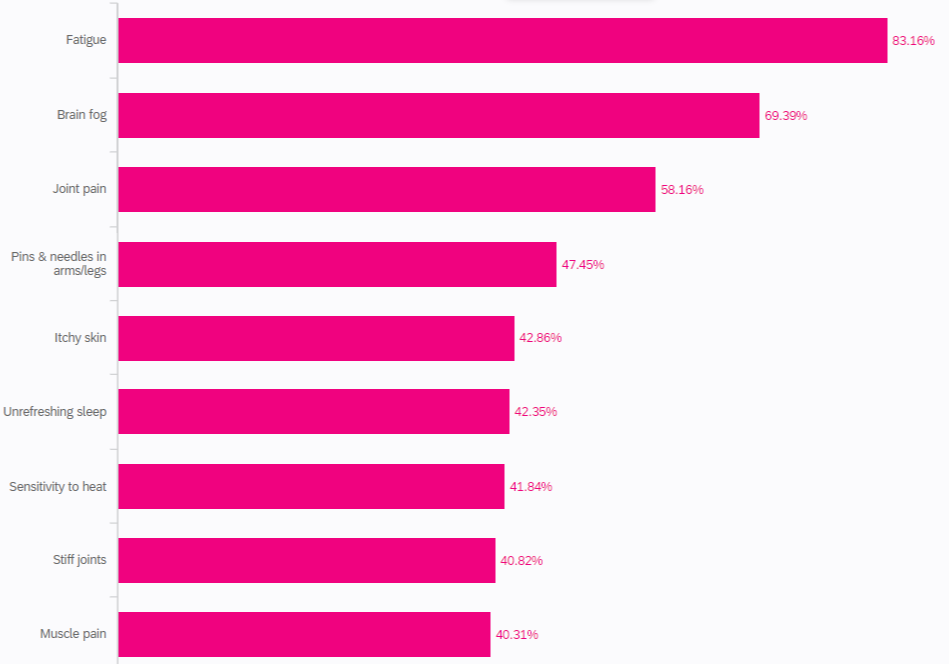
Overall, the most common symptoms reported were fatigue, brain fog, and joint pain, with 83% of survey takers reporting fatigue, 69% brain fog, and 58% joint pain.
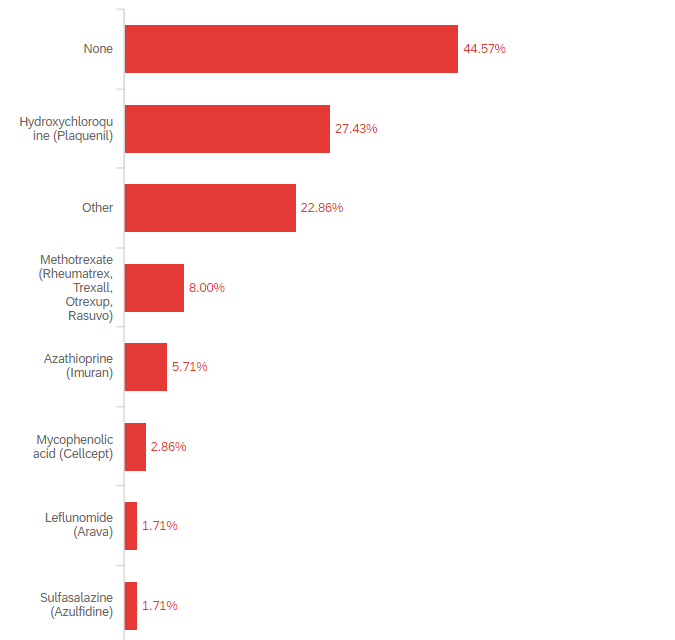
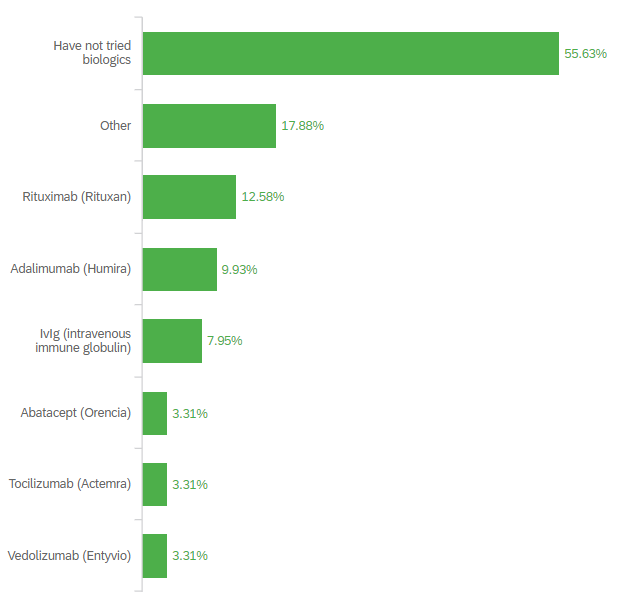
When it comes to medications, we found that 27% of patients are taking plaquenil, 8% methotrexate, and 6% Imuran, while 45% are not taking any type of disease modifying rheumatic medications (DMARDS). When it comes to Biologics, 56% reported never having tried this type of treatment, with the most common Biologic treatment received being Rituxan 14%, followed by Humira 10% and IVIG (Intravenous Immunoglobulin) 7.95%.
Do you have a question about the survey for your particular disease? Let us know and we will look up the information from the survey results.
With more members in our registry, we can generate these types of statistics on a larger scale. Please join our registry or share it with a friend who has an autoimmune condition. Donations are also greatly appreciated!